Healthcare workers have to deal every day with the risks that may arise from handling fluids produced by the human body, with the main examples being blood, urine, feces and sputum. These
fluids may pose a health risk due to the potential presence of pathogens and/or residues of cytotoxic products used in chemotherapy treatments.
In addition to the risk of exposure to bodily fluids through injury (cuts or needle pricks) (INSPQ,
2019), there is a risk of spattering when a worker is handling or transporting equipment containing
bodily fluids. Also, in some cases, there is a risk of contamination when disposing of these fluids in
a toilet. This risk can stem from the creation of droplets and aerosols when the toilet is flushed. For
example, one study showed the presence of a virus population in the air after a single flush (Cooper
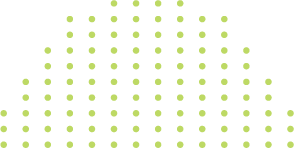
2017). In this study, the researchers also quantified the virus population in the air over certain periods of time. The results, as shown in Figure 1, indicate that concentrations remain relatively high
for the first 15 minutes and that there is a potential risk up to one hour after flushing, depending on
ambient conditions and the nature of the infectious dose (Cooper, 2017).
The risk associated with handling body fluids is very high
A virus (such as the gastroenteritis virus) could therefore be inhaled or could end up on a surface,
presenting a risk of contamination through indirect contact. As mentioned above, bodily fluids
may also be contaminated by residues of cytotoxic products used in chemotherapy treatments
(Fransman, 2007). Workers’ exposure to these products can be from inhalation or from contact
(direct or indirect) with the skin or the mucous membranes (Sessink et al., 2015). The ASSTSAS prevention guide (2008) reports that, “of 18 studies, 16 detected the presence of drugs in the urine of
staff members, four of whom did not handle drugs.” The authors of the document believe that, for
these four people not handling products, the source of contamination is indirect, through contact
with contaminated surfaces.
Exposure to cytotoxic products may cause various pathologies among workers. According to an
alert issued by the National Institute for Occupational Safety and Health (NIOSH) in 2004, it may
cause infertility, skin rashes, miscarriages, birth defects and, possibly, various cancers. It is important to remember that, in addition to healthcare workers, people working in veterinary hospitals are
also exposed to these types of drugs.
Besides the risk associated with preparing drugs, the handling and transportation of bodily fluids
presents a risk of spattering or spillage that may lead to exposure through direct contact with hazardous drugs. For example, studies have indicated a risk of exposure in the handling of patients’
urine when it is flushed down toilets (Kromhout et al., 2000, Fransman et al., 2007). Also, these drugs
may hypothetically be found in droplets and aerosols when flushing.
Exposure to bodily fluids may occur in various units in a hospital, depending on the activities being
performed there. Operating rooms are a good example of this. Bodily fluids produced during surgery put workers at risk throughout the waste-management process (Larocque et al., 2017). Fluids
from irrigation alone may produce nearly 1,282 ml of liquid on average (Larocque et al., 2017). It
should be noted that volumes vary according to the type of surgery. In light of these examples, reducing the risk from handling bodily fluids is vital in ensuring the health and safety of healthcare
workers. At present, other than vaccination and simple basic practices such as washing hands,
wearing gloves and gowns and protecting the eyes, there are few techniques for reducing the risk
from handling bodily fluids to meet the needs of various healthcare activities. Operating rooms
do offer the possibility of using a closed exhaust system (UETMIS, 2018). However, large volumes of
bodily fluids (10 litres or more) would have to be produced for this equipment to be economically
advantageous (Larocque et al., 2017).
The current open system therefore remains the main alternative for all care units in managing bodily fluids, despite the significant risk it poses to workers. But there are ways to improve the open
system so as to reduce risk exposure. One such possibility is the use of hygienic bags with an absorbent pad for urine, vomit and liquid stools. Another is the use of ultra-absorbent sticks that can
absorb a litre or more of fluids. They simply need to be inserted in the container to cause the liquid
to gel (examples include suction containers and urine collection containers). This substantially limits workers’ risk of exposure to bodily fluids.
By extension, it also limits the socio-economic costs of a worker developing a pathology. It should
be noted that this type of stick may also be used to deal with small spills in the surroundings.
By Richard Massicotte, PhD
RÉFÉRENCES :
Association paritaire pour la santé et la sécurité du travail du secteur affaires sociales (ASSTSAS), 2008. Guide de prévention; Manipulation sécuritaire des
médicaments dangereux. 158 p.
Cooper J., 2017, The role of hospital toilets in microbial dissemination and the effectiveness of ultraviolet C irradiation, Thesis, University of British Columbia,
104 p. Fransman W, 2007. Antineoplastic drugs: Occupational exposure and health risks , Thesis Utrecht University 168 p. Institut Nationale de Santé Publique du Québec (INSPQ), 2019, Exposition aux liquides biologiques, https://www.inspq.qc.ca/sante-voyage/guide/risques/liquides-biologiques/definition.
Kromhout H, Hoek F, Uitterhoeve R, Huijbers R, Overmars RF, Anzion R, Vermeulen R. 2000. Postulating a dermal pathway for exposure to anti-neoplastic
drugs among hospital workers. Applying a conceptual model to the results of three workplace surveys. Ann Occup Hyg 44:551-560. Kromhout H, Hoek F,
Uitterhoeve R, Huijbers R, Overmars RF, Anzion R, Vermeulen R. 2000. Erratum to: «Postulating a dermal pathway for exposure to anti-neoplastic drugs
among hospital workers. Applying A conceptual model to the results of three workplace surveys». Ann Occup Hyg 44:657. Larocque B., L’Espérance S., Nourissat A.,Coulombe M., Rhainds M., 2018, Évaluation d’un système en circuit fermé pour la gestion des déchets liquides biologiques au bloc opératoire dans
le cadre des travaux du Nouveau complexe hospitalier du CHU de Québec-Université Laval. Sessink P. J.M., Sewell G. Vandenbroucke J., 2015. Preventing
occupational exposure to cytotoxic and other hazardous drugs. Policy recommendations. Editor: Amaya Erce, Rohde Public Policy, 28 p. The National Institute for Occupational Health and Safety (NIOSH),2004. Alert, Preventing Occupational Exposures to Antineoplastic and Other Hazardous Drugs in Health
Care Settings. Department of health and human sciences, Centers for disease control and prevention (CDC), 58 p. Unité d’évaluation des technologies et des
modes d’intervention en santé (UETMIS)2018, Rapport d’évaluation 10-18, Direction de la qualité, de l’évaluation, de l’éthique et des affaires institutionnelles
(DQEEAI), préparé par : FRCPC UETMIS, CHU de Québec-Université Laval https://www.chudequebec.ca/professionnels-de-la-sante/evaluation/evaluation.
aspx, 69 p.